
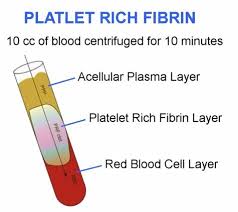
PRF is useful in bone grafting and dental implants because it helps the body heal faster, promotes better bone and gum tissue growth, reduces the risk of infection, and decreases pain and swelling after dental surgical procedures. It is made from the patient’s own blood which ensures it is safe and biocompatible with the body. Platelet-Rich Fibrin helps with healing in procedures such as bone grafting and dental implants. The blood sample is taken from the patient immediately before the procedure and put in a centrifuge for 8-12 minutes.
PRF platelet rich fibrin
PRF offers several advantages:
- Faster healing: PRF has special elements called growth factors, which speed up the healing process by helping cells move, grow, and change in the body.
- Better bone growth: The growth factors in PRF help new bone form more quickly and improve the quality of the bone graft, which is important for dental procedures.
- Improved soft tissue healing: PRF helps the soft tissues around the dental implant or bone graft heal faster by reducing inflammation and promoting the growth of new blood vessels.
- Lower chance of infection: PRF can help fight against infections during and after dental procedures because it has natural germ-fighting properties.
- Less pain and swelling: After dental procedures, patients often experience pain and swelling. PRF can help reduce these symptoms, making the healing process more comfortable.
- Made from the patient’s own blood: Since PRF is made from the patient’s blood, there’s no risk of catching diseases from someone else’s blood or having an allergic reaction. This means the body is more likely to accept PRF and heal well.
How PRF bone grafting works
PRF is extremely beneficial in bone preservation, formation and new bone deposition around newly placed dental implant sites. Platelet rich fibrin, also called PRF greatly enhances and accelerates the biological process of growing bone around the surface of implants and jaw bone tissues. Successful implant healing is achieved in the presence of platelet rich fibrin which is the first and foremost step for the success of tooth replacement.
PRF helps bone defects regenerate and heal. Especially around front teeth and areas of greater esthetic concern. Platelet rich fibrin helps bone regeneration and helps in filling the defects to facilitate excellent outcomes in a short amount of time. PRF remains active in the surgical site for approximately 14-28 days as compared to 14 hours duration of platelet rich plasma.
PRF Bone Graft Technique Video:
Why is Platelet Rich Fibrin used for Implants?
- Less swelling and pain after dental implant procedure
- Faster healing of bone around dental implants
- Stronger bone integration to dental implants
- Decreases chances of infection after implant surgery
- Decreases chances of implant failure
- Helps prevent bone loss around implants
- Preserved bone around tooth extraction sites
Contact Dr. Adams for a complimentary implant consultation including 3D Xray
What is PRF or Platelet Rich Fibrin?
Platelet rich fibrin dramatically increases implant surgery success rates. In addition to increasing the quantity of bone in the required dimensions, it also enhances gum tissue growth and regeneration following dental implant placement. Deposition of cementum-like tissues has been associated with platelet rich fibrin further making dental implants mimic natural teeth roots. Platelet rich fibrin has been considered as the gold standard in all procedures involving indications for bone and soft tissue regeneration and imparting beautiful smiles in areas requiring larger bone fills is quite possible now. PRF helps oral surgeons with wisdom tooth extraction sites. It facilitates at an accelerated rate. And it also reduces the risk of infection.

PRF dental platelet rich fibrin 1
Platelet Rich Fibrin Preserves Bone in Extraction Sites
Successful dental implant surgery requires sufficient thickness, quality, width and quantity of healthy jaw bones in the intended socket area following loss of natural teeth. Resorption and loss of socket bone following removal of compromised natural teeth is common and approximately 1/4th of the bone around empty sockets diminishes in the first year after tooth removal. Immediate implant placement has been documented to be a successful method for preventing these unwanted consequences but cannot always be performed. Similarly, socket preservation methods leaving some portion of the root within the jaw bones have also shown less bone dissolution. Recent innovations have given rise to autologous platelet concentrates which have shown promising results. Platelet rich plasma has been in common practice for bone and soft tissue regeneration and preservation but it showed lesser efficacy and the need for an activator and associated coagulopathies due to presence of bovine thrombin limited its use.
Other Popular Blog Posts:

 (301) 421 1996
(301) 421 1996 burtonsvillesmiles@gmail.com
burtonsvillesmiles@gmail.com